Introduction:
EOL care in patients (pts) with hematologic malignancies (HM) has been inadequately studied. Available data suggest that pts with HM are more likely to be hospitalized and receive chemotherapy at EOL, and less likely to be enrolled in hospice relative to pts with solid tumors. Better understanding of the barriers to high-quality EOL care is needed for HM pts. The aim of this study was to identify potential barriers to high-quality EOL care for pts with AML and MDS.
Methods:
We conducted a retrospective study of pts aged ≥18 years with AML or MDS who were evaluated at Wilmot Cancer Institute and its affiliates, and died between Jan 1, 2014 and Dec 31, 2019. We collected the following EOL metrics: 1) Hospice enrollment; 2) Palliative care (PC) referral; 3) MOLST form completion and do-not-resuscitate orders; 4) Chemotherapy administration within the last 14 days of life; 5) Utilization of the emergency department (ED), hospital, intensive care unit (ICU), and life-sustaining treatments (LSTs) within the last 30 days of life; 6) Transfusion within the last 7 days of life; 7) Place of death; and 8) Time from MOLST form completion, PC referral, and hospice enrollment to date of death. Fisher's exact tests were used to compare EOL metrics between pts with MDS and AML. We used cumulative incidence functions to estimate the probability of PC referral and MOLST form completion within 12 weeks of the first hematology visit, accounting for the competing risk of death. We analyzed the univariate and multivariate associations of timing (>30 days vs never/30 days prior to death) of MOLST form completion, PC referral, and hospice enrollment with utilization of the ED, hospital, ICU, and LSTs at EOL. We evaluated the associations of MOLST form completion, PC referral, and hospice enrollment with hospital death.
Results:
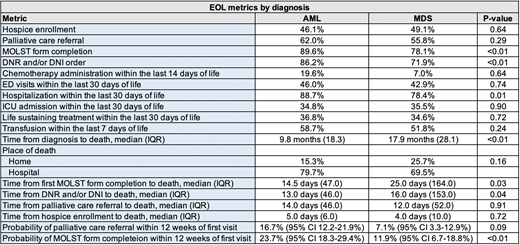
We included 120 pts with MDS (mean age 73.6; range 25-93) and 238 pts with AML (mean age 65.7; range 20-95). EOL metrics by diagnosis are shown in Table 1.
The probability of PC referral within 12 weeks of the first hematology visit was 16.7% [95% Confidence Interval (CI) 12.2-21.9%] and 7.1% (95% CI 3.3-12.9%) for AML and MDS, respectively. The probability of MOLST form completion within 12 weeks of the first hematology visit was 23.7% (95% CI 18.3-29.4%) and 11.9% (95% CI 6.7-18.8%) for AML and MDS, respectively.
A MOLST form was completed early (>30 days before death) in 33.3% (N=115/345) of pts. In univariate analysis, these pts were less likely to be hospitalized (78.1 vs 89.3%, p<0.01), be admitted to the ICU (13.9 vs 45.1%, p<0.01), and to utilize LSTs at EOL (13.9 vs 46.7%, p<0.01). Early hospice enrollment (>30 days before death) occurred in 3.8% (N=13/340) of pts. In univariate analysis, these pts were less likely to visit the ED (0 vs 46.6%, p<0.01), be hospitalized (26.7 vs 87.9%, p<0.01), be admitted to the ICU (0 vs 36.5%, p<0.01) and to utilize LSTs at EOL (0 vs 37.5%, p<0.01). Early PC referrals (>30 days before death) occurred in 21.4% (N=73/341) of pts and was not associated with EOL metrics in univariate analysis.
In multivariate analysis, after adjusting for age and diagnosis, early MOLST form completion was associated with a lower risk of ICU admission [Odds Ratio (OR) 0.23, p<0.01] and lower risk of utilization of LSTs (OR 0.21, p<0.01). Early hospice enrollment was associated with a lower risk of ED visitation (OR 0.04, p=0.03) and hospitalizations (OR 0.05, p<0.01). Hospice enrollment at any time was associated with a lower risk of death in the hospital (OR 0.14, p<0.01), while MOLST form completion (OR 5.26, p<0.01) and PC referral (OR 4.44, p<0.01) were associated with a higher risk of death in the hospital (likely reflecting the fact that many were done close to EOL in the hospital). There was not a significant association between early PC and EOL metrics in multivariate analysis.
Conclusion:
We found a high rate of ED visits, hospitalizations, ICU admissions, and use of LSTs at EOL in pts with MDS and AML. The majority of these pts died in the hospital. While most patients completed MOLST forms and had palliative care referrals, these events generally occurred very late in the disease course, often close to EOL. Early MOLST form completion and early hospice enrollment were associated with better EOL quality metrics. Interventions to promote timely completion of orders for life-sustaining treatment, PC referrals, and hospice enrollments may improve EOL care among pts with AML and MDS.
Loh:Pfizer: Consultancy; Seattle Genetics: Consultancy. Liesveld:Abbvie: Honoraria; Onconova: Other: data safety monitoring board. Aljitawi:Sanatela Medical: Patents & Royalties: Patent pending. Mendler:Jazz Pharmaceuticals: Speakers Bureau; GLG: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.